Varicose veins are more than a cosmetic nuisance—they can cause aching, swelling, and long-term complications that interfere with work and daily life. For individuals who spend long hours managing websites, outreach campaigns, or client accounts, prolonged sitting and stress can increase the risk of vein-related issues.
This article, written for busy online entrepreneurs and SEO professionals, outlines practical and evidence-informed solutions for maintaining leg health. It covers what causes varicose veins, when to seek medical care, effective at-home strategies, minimally invasive treatments, advanced surgical options, and long-term prevention. It also highlights the importance of consulting a qualified vein specialist near Sunset Hills to ensure timely diagnosis and personalized treatment, helping readers address vein problems early and choose the most effective care path.
What Causes Varicose Veins and Who is at Risk?
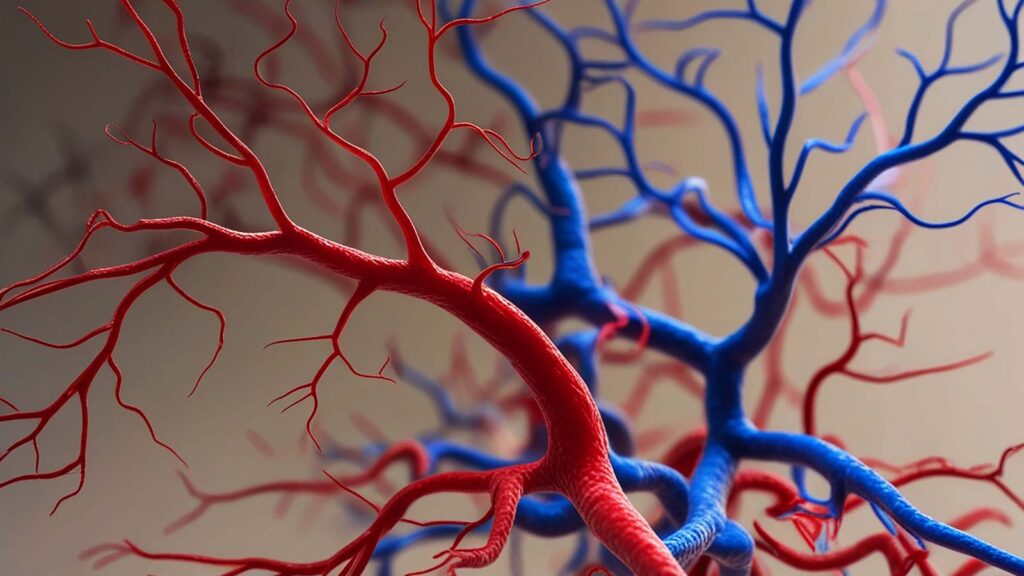
Varicose veins form when veins, most commonly in the legs, fail to move blood efficiently back toward the heart. Veins contain one-way valves that prevent backflow. When those valves weaken or are damaged, blood pools, the vein stretches, and the familiar bulging, twisted appearance develops. Several factors increase the chance that veins will become varicose.
Common Risk Factors
- Age: Vein walls and valves weaken over time; risk rises after age 40.
- Genetics: Family history is one of the strongest predictors; if parents had varicose veins, their children are more likely to get them.
- Sex and hormones: Women are affected more often than men. Hormonal changes during pregnancy, menstruation, and menopause can relax vein walls.
- Pregnancy: Increased blood volume and pressure from the uterus can temporarily worsen or reveal varicose veins.
- Prolonged standing or sitting: Jobs requiring long periods upright or seated, like managing e-commerce operations, doing outreach, or working at a desk, raise risk due to reduced calf-muscle pumping.
- Obesity: Extra weight increases venous pressure in the legs.
- History of blood clots or leg trauma: Prior deep vein thrombosis (DVT) or injury can damage venous valves.
How Vein Anatomy Leads to Symptoms
When venous valves fail, blood refluxes downward under gravity. This causes increased pressure in superficial veins, stretching them and making them visible. The pressure and pooling trigger inflammation of surrounding tissues, which explains common symptoms: aching, heaviness, cramping, restless legs at night, swelling (edema), and skin changes. In advanced cases, chronic venous insufficiency can produce brownish skin discoloration or venous ulcers. Understanding the anatomy clarifies why treatments aim either to restore valve function, remove dysfunctional veins, or redirect blood flow through healthier channels.
Symptoms, When to Seek Medical Evaluation, and Tests
Recognizing symptoms and knowing when to get evaluated helps avoid complications. Many people start with cosmetic concerns, but the presence of physical symptoms or skin changes warrants prompt assessment.
Warning Signs that Require Prompt Care
- Rapidly worsening pain, swelling, or redness in a leg (possible DVT).
- Persistent, progressive swelling that doesn’t resolve with elevation or compression.
- Skin changes: darkening, hardening, or eczema-like rashes over the lower leg.
- Non-healing sores or ulcers around the ankle or lower leg.
- Sudden onset of significant warmth and tenderness along a superficial vein (superficial thrombophlebitis).
If any of these occur, people should seek medical attention promptly: DVT in particular requires urgent evaluation.
Conservative At-Home and Lifestyle Treatments
Many patients benefit significantly from nonprocedural measures. These options are low-risk, can be started immediately, and often reduce symptoms while improving overall leg health.

Compression Therapy: Types and Proper Use
Compression stockings are the cornerstone of conservative management. They apply graduated pressure (stronger at the ankle, decreasing toward the thigh) to assist venous return. Options include:
- Over-the-counter support stockings (mild compression, 8–15 mmHg) for mild symptoms.
- Medical-grade compression (15–20, 20–30, 30–40 mmHg) is available by prescription for more pronounced swelling and symptoms.
Proper fit is crucial; stockings that are too tight at the calf or thigh can be uncomfortable and ineffective. People should try them on in the morning before swelling starts and follow the manufacturer’s sizing or the clinician’s guidance. Consistent daily wear during active hours provides the best symptom relief.
Exercise, Weight Management, and Elevation Techniques
Movement engages the calf-muscle pump, a natural venous booster. Simple, practical habits help:
- Walk regularly: short walks every hour break, and extended sitting.
- Calf raises and ankle pumps: ten repetitions several times a day improve circulation and are easy to do at a desk.
- Weight reduction: even modest weight loss lowers venous pressure and symptom burden.
- Leg elevation: elevating legs above heart level for 15–30 minutes daily reduces swelling. Do this after work or long sitting periods.
For online entrepreneurs managing client work, setting an hourly alarm to stand, stretch, and walk 2–3 minutes is a small change with outsized benefits.
Skincare, Pain Relief, and Symptom Management Tips
Good skin care prevents complications: moisturize dry skin, avoid tight bands at the knee that can constrict flow, and inspect skin daily for changes. Over-the-counter anti-inflammatory meds can reduce discomfort for short periods: topical analgesics and cold compresses offer temporary relief. Smoking cessation and controlling blood pressure and diabetes also support vascular health. If symptoms persist even though these measures are taken, or if cosmetic concerns are significant, evaluation for procedural options is reasonable.
Minimally Invasive Procedures: What to Expect
Minimally invasive treatments have largely supplanted open surgery for most patients with symptomatic varicose veins. These procedures target the source of reflux and permit quicker recovery.
Endovenous Ablation (Laser or Radiofrequency)
Endovenous thermal ablation uses heat, delivered by laser (EVLA) or radiofrequency (RFA), to close the incompetent saphenous vein. The process generally follows this pathway:
- Local anesthesia plus light sedation if needed.
- Ultrasound-guided insertion of a catheter into the affected vein.
- Delivery of thermal energy to collapse and seal the vein, rerouting blood through healthy deep veins.
Most patients can walk out the same day and return to normal activities within a few days. Compression stockings are typically worn for 1–2 weeks. Success rates are high, with relief from aching and reduced recurrence compared with conservative care alone.
Sclerotherapy for Smaller Veins
Sclerotherapy involves injecting a sclerosant (chemical irritant) into spider veins or smaller varicose veins, causing them to collapse and fade. Foam sclerotherapy treats somewhat larger veins. Treatments are quick, done in-clinic, and may require multiple sessions spaced weeks apart. Mild bruising and temporary discoloration are common; significant complications are rare when performed by experienced clinicians.
Procedure Recovery, Risks, and Typical Outcomes
Recovery from minimally invasive vein procedures is generally fast. Common, expected short-term effects include soreness, bruising, and mild nerve irritation along treated areas. Serious complications, deep vein thrombosis, skin burns, or persistent numbness, are uncommon but discussed during informed consent. Long-term outcomes show symptom improvement in most patients and cosmetic benefits for many, but new veins can develop over time, and maintenance strategies may be necessary.
Surgical and Advanced Options for Severe Cases
When disease is extensive or when anatomy doesn’t suit endovenous techniques, surgical approaches remain valuable. Advanced options are tailored to disease severity and patient needs.
When More Invasive Surgery is Recommended
More invasive surgery may be recommended when:
- Extensive venous reflux involves complex superficial and deep systems that can’t be managed with endovenous tools.
- Prior interventions have failed, or there is recurrent disease that requires anatomical correction.
- Large venous aneurysms or severe skin breakdown/ulceration need direct surgical attention.
A vascular surgeon or phlebologist will review imaging and symptoms to formulate an individualized plan. Multimodal treatments, combining ablation, phlebectomy, and conservative care, are common and often deliver the best functional and cosmetic results.
Preventing Recurrence and Long-Term Leg Health
Treatment doesn’t always mean the end of vein concerns; proactive maintenance reduces recurrence and preserves leg health over time.
Maintenance Strategies and Lifestyle Modifications
- Continue compression use during long travel or periods of prolonged standing/sitting.
- Maintain regular leg exercise: walking, cycling, and calf-strengthening.
- Manage weight, blood pressure, and blood sugar to reduce vascular stress.
- Avoid tight clothing that compresses the groin or behind the knee for extended periods.
- For people with hormonal risk (e.g., pregnancy plans), discuss the timing of elective procedures with a clinician: pregnancy can cause new or worsened veins.
Online professionals should integrate movement into workflows, standing meetings, a walking call, or scheduled stretch breaks to reduce venous strain.
Follow-Up Care and When to Re-Evaluate
After procedural treatment, scheduled follow-up and periodic duplex ultrasound help confirm lasting closure of treated veins and detect new reflux early. People should re-evaluate with a clinician if symptoms return, swelling increases, or skin changes appear. Long-term surveillance is especially important when prior deep vein thrombosis exists or when chronic symptoms persist even after intervention.

Conclusion
Effective varicose vein solutions for leg health range from lifestyle changes and compression to highly effective minimally invasive procedures and selective surgery. Early recognition, appropriate diagnostic ultrasound, and a tailored treatment plan produce the best outcomes. For busy online entrepreneurs, affiliate marketers, and agency professionals, simple habits, hourly movement, proper compression during long flights, and prompt evaluation of worsening symptoms protect productivity and long-term leg health. When symptoms persist or impair daily life, consulting a vascular specialist ensures conservative measures and procedural options are weighed against individual goals and risk. Investing a little time in prevention and timely treatment can preserve comfort, mobility, and the ability to keep work moving forward.